No products
To be determined
Shipping
0,00€
Total
Product successfully added to your shopping cart
Quantity
Total
There are 0 items in your cart.
There is 1 item in your cart.
Total products
Total shipping
To be determined
Total
The right size of dental implant is the key to long-term osseointegration
The choice of the implant diameter influences its primary stability, successful osseointegration, as well as foresees a risk of atrophy around the implant. The diameter is directly dependent on crestal bone characteristics, its thickness and bone quality. The implant is to be all round surrounded with bone, which thickness exceeds 0.75-1.0 mm. When selecting the diameter, consider the distance between adjacent teeth and medio-distal tooth size. Each case requires individual calculation.
The correct implant selection
1. Increases bio-cortical primary stability.
2. Provides larger surface area for osseointegration.
3. Contributes to a more axial orthopedic oriented position of the whole construction.
Frequently, when bottom or upper jaws lack one molar, doctors deal with the issue of a required number of placed implants: one or two. At a distance of 10 mm between interproximal areas of teeth adjacent to implantation site, one implant is placed. Platform width is chosen depending on the distance. In case inter-aproximal distance exceeds 14 mm, placing of two implants is recommended. At a distance of 10-14 mm, the situation becomes most controversial. In this case, adequate width allows placing of one wide implant (5 or 6 mm diameter) or two narrow implants (3.4 mm diameter), with narrow crestal bone.
In addition to inter-aproximal distance, doctors mind the distance between root sections of teeth adjacent to implantation site, as well as the root section angulation towards the dental crown axis.
Biomechanics of dental implants: diameter and length
Chuiko A.N. and Kholin D.E. researched biomechanics of implants and made proper calculations. Let's see an example of these calculations.
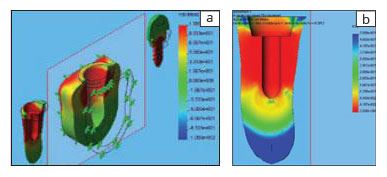
Red zone corresponds to FOS <0,05, - blue zone - FOS> 0,5. In this example, calculated allowance δ = 1 mm leads to tensions, which significantly exceed traumatic bone tension.
Von Mises stress field in all system elements (a), margin of safety coefficient field for (b)
Conclusions
1. Confirmed by means of finite-element modeling, preliminary analysis (at basic mechanic relations) shows that support portion of the implant, influenced by mastication load, creates two zones of stress concentration: in the implant collar and lower implant end areas.
Given the facts the value of mastication load (along with action distance) is practically fixed and mechanical properties of a specific patient's bone tissue (firstly traumatic stress) tend to vary within a small range, the only way to reduce stress in concentration zones is their rational distribution by optimizing the implant design.
2. In mathematical terms, consideration of the jaw anatomical and topographical features, that is availability of "free" space for placing the implant, is a necessary condition. Provision of actual bone stress field that not exceeds the value of traumatic stress is a sufficient condition.
Thus, a conventional requirement for implantation on necessary bone quantity and quality is updated with a specific content: one can determine the thickness of structural bone components, in which the implant dimensions can be maximized. With precisely known properties of a patient's bone tissue, the result is even more proved.
Considering a proposed need to approximate the implant anchorage area to the root area of replaced teeth, there's an opinion saying that starting implant of largest possible diameter is to create favorable conditions in terms of stress distribution. In this case, primary fixation proceeds more favorable, while reimplantation is not required.
3. The implant's taper in collar area, with optimal sizes, helps distribute mastication load in the most rational way.
Compared to a cylindrical implant under 100% osseointegration, the screw implant (screw joint) features no significant advantages. However, it is technically more sophisticated, while increasing the surgery injury rate through developing zones of stress concentration.
4. Back taper collar prevents resorption of crystal bone and provides steadier attachment of mucosa around the collar.


